Support that’s more than medicine.
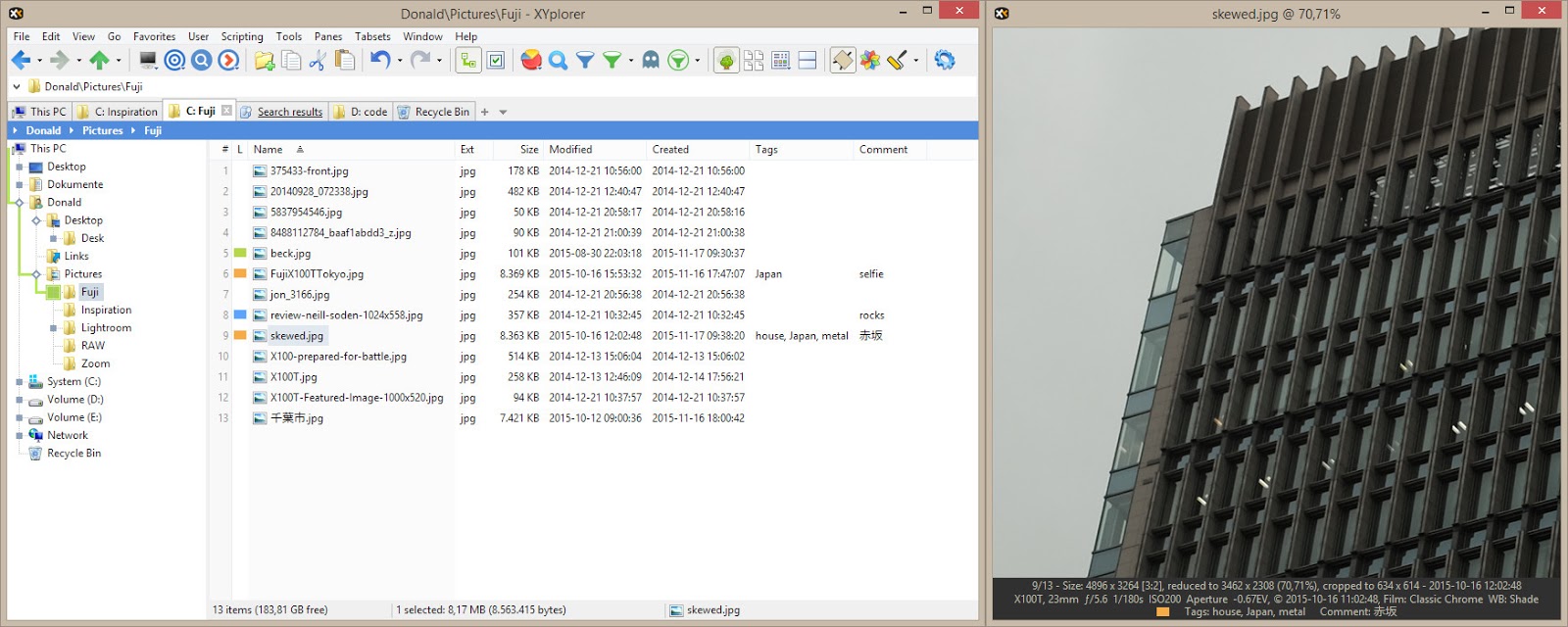
- Xyplorer Scripts Express Members Sign In
- Xyplorer Scripts Express Membership Cost
- Xyplorer Scripts Express Membership
Express Scripts is the country’s largest pharmacy benefit manager and one of the largest pharmacies. Now, as always, we’re here to help.
- Simple, stress-free ordering
- Safe, accurate prescriptions delivered to your door
- World-class customer support, 24x7
Express Scripts resources for pharmacists. Read latest notifications, file pricing appeals and search Express Scripts claims and patient coverage for your Pharmacy customers. A growing team of more than 500 pharmacy pricing, contract, service, technology, data, and clinical experts that work together as one team towards one common goal: putting the benefit back in pharmacy benefits.
Already have an account? Log in
Stay Safe with Home Delivery
Skip the trip to the pharmacy. We'll send medication right to your door so you can stay safe.
COVID-19 Resource Center
Check out the latest COVID-19 vaccine news and learn more about when and how to sign up.
Shipping Alert
Deliveries may be delayed due to increased shipping demand.
Express Scripts® Pharmacy is all about you.
Your health and safety is our top priority and at the heart of what we do. Whether you’re a longtime customer of the Express Scripts® Pharmacy or you turned to us recently during the COVID-19 pandemic, we’re here to serve you, 24/7.
Our commitment to you is stress-free prescription management, reliable delivery, and world-class pharmacy care from specially-trained pharmacists. If you ever have a question about your medication or order, give us a call or send us a note. We’re here to help.
Wendy Barnes
President, Express Scripts® Pharmacy
Learn more about
Express Scripts® Pharmacy

Safely manage your medication from home.
With over 1 million downloads, the Express Scripts® mobile app puts all your pharmacy needs within reach. Download today from your device's app store.
Healthcare can be complicated. That’s why our experts are available 24/7.
We're always here to give you the information and support you need to take control of your health. Want to know more about how we make it easier to manage your medication?
Millions of Americans have lost coverage. We can help.
Express Scripts Parachute Rx℠ makes prescription medications affordable if you are uninsured. Find discounts on thousands of generic and brand-name drugs.
Get more from your Express Scripts benefits.
Already have an account? Log in.
Medicare Part D Formulary (drug list)
A formulary is the list of drugs covered by a Part D plan. Medicare requires all Part D plans to cover at least two drugs in each therapeutic drug category.
Express Scripts Medicare plans typically cover the drugs listed in the formulary, as long as:
- The drug is medically necessary
- The prescription is filled at one of our network pharmacies
- Any special drug coverage rules are followed, as required
Some types of drugs are not covered by Medicare Part D, such as drugs for weight loss or cosmetic purposes.
The level of coverage for each drug will depend in part on which tier the drug is in. You can find more information about drug tiers in the Evidence of Coverage and formularies listed below.
Tier 1 Preferred Generic Drugs
Tier 2 Generic Drugs
Tier 3 Preferred Brand Drugs
Tier 4 Nonpreferred Drugs
Tier 5 Specialty Tier Drugs
Tier 6 Select Care Tier Drugs (Value and Choice plans only)
NEW! Part D Seniors Savings Model
Express Scripts Medicare offers insulin at an affordable and predictable price with our Saver and Choice plans. You will pay $35 or less for select insulin medications from any network pharmacy, in all stages up to the Catastrophic Coverage Stage. View a list of the included drugs. If you receive 'Extra Help,' you do not qualify for this program, and your Low-Income Subsidy copay level will apply.
To view and/or print our formulary now, click on the plan option below:
You may also access our online searchable tool to confirm if your drugs are covered and to see if there are any special coverage rules.
To request a comprehensive formulary be mailed to you, send an email with your full name, phone number and mailing address to documents@express-scripts.com. For assistance, call 1.866.477.5703, 8 a.m. to 8 p.m., 7 days a week, except Thanksgiving and Christmas. TTY users, call 1.800.716.3231.
Special drug coverage rules
Some drugs have special coverage rules that may:
- Limit the amount of a particular drug you can get
- Require that you get prior approval from the plan before a drug is covered (known as prior authorization)
- Require that you first try a certain drug to treat your condition before another drug is covered (known as step therapy)
- Limit which pharmacies you can use
Drugs that are subject to these rules are clearly marked in the formulary.
View the list of prescription drugs that currently have prior authorization or step therapy requirements and the rules that apply to each drug:
Saver plan
Value plan
Xyplorer Scripts Express Members Sign In
Choice plan
Once coverage begins, you may request an exception to our coverage rules. Learn more about exceptions and appeals.
Formulary changes
Express Scripts Medicare plans may periodically:
- Add a drug to or remove a drug from the Drug List
- Move a drug to a higher or lower cost-sharing tier
- Add or remove a restriction on coverage for a drug
- Replace a brand-name drug with a generic drug
If we make certain changes to our formulary for a drug you are taking, we will either notify you at least 30 days before the change is made or notify you after the change is made and give you a 30-day refill of the drug at a network pharmacy.
Xyplorer Scripts Express Membership Cost
If the U.S. Food and Drug Administration finds that a drug on the formulary is unsafe, or if the drug's manufacturer removes the drug from the market under Medicare Part D regulations, we immediately remove the drug from our formulary and then notify you of the change.
Xyplorer Scripts Express Membership
For additional information on formulary changes, please review Chapter 3 of the Evidence of Coverage.